Family Medicine
Sat 27th/Sun 28th March 2021
INTERYem and Family Medicine
The provision of comprehensive and coordinated care between primary and secondary care services in Yemen through the effective use of FM can promote patient engagement, reduce costs to patients and increase wellbeing in society. The provision of services that are coordinated, rather than being constrained to an individual disease or organ system, provides a basis for the holistic approach to chronic illness and multimorbidity in Yemen provided through FM.
Where FM healthcare professionals (HCPs) are based in, and known to, their local community, this provides an opportunity to develop trust between such HCPs, patients and the wider community. In such a situation, patients are more likely to engage with HCPs who are known and trusted during a long-term illness; hence, they are more likely to seek health interventions earlier (with better patient outcomes and lower financial burdens), and to be open to preventive medicine.
Despite the benefits of an effective FM system described above, much of the public in Yemen (as with other countries) still believes FM to be inferior to secondary care, particularly regarding disease-specific treatment. There are many reasons for such misperceptions, including: FM HCPS have smaller budgets than in secondary care, and so have fewer resources to treat their patients with, hence the potential for poorer health outcomes; a belief that diagnostics is necessary for high quality clinical practice, and a relegation of the importance of history and examination; and that a generalist is likely to be inadequately trained relative to a specialist. Despite acknowledging that multi-levelled healthcare system is key to success and efficiency, health services in Yemen remain skewed towards specialist care.
There is evidence to suggest that FM and economic development are linked in lower countries such as Yemen. If the Yemen health system were to utilise FM effectively, it is likely to have lower health-to-cost ratios, and more equitable health outcomes. However, many of the advantages of FM may not be clearly distinguishable to policy-makers and may be eclipsed by secondary care solutions; in the post-conflict Yemen, it would be tempting for health policy makers to seek more obvious and expensive health interventions over evidence-based and less glamourous interventions such as those delivered via FM.
Challenges
For Yemen, the challenges of high chronic disease rates, poor infrastructure, low- and high-level conflict, and patients’ lack of experience of secondary care demonstrate opportunities for FM. By integrating FM solutions, Yemen could emulate health systems such as those of UK, Cuba and Brazil, and its neighbour Oman, in developing efficient but effective health structures.
As education, training and research in FM seemingly remain a low priority for Yemen’s health policy makers, despite clear socio-economic and health benefits, this is a field that INTERYem (the International Network for Training, Education and Research for Yemen) believes should be focussed on as one of the priority areas for the foreseeable future.
INTERYem has as its three founding objectives for HCPs:
01 Education
02 Training
03 Research
For Yemen, the challenges of high chronic disease rates, poor infrastructure, low- and high-level conflict, and patients’ lack of experience of secondary care demonstrate opportunities for FM. By integrating FM solutions, Yemen could emulate health systems such as those of UK, Cuba and Brazil, and its neighbour Oman, in developing efficient but effective health structures.
As education, training and research in FM seemingly remain a low priority for Yemen’s health policy makers, despite clear socio-economic and health benefits, this is a field that INTERYem (the International Network for Training, Education and Research for Yemen) believes should be focussed on as one of the priority areas for the foreseeable future.
INTERYem has as its three founding objectives for HCPs in YemenEducation, Training, and Research.
List of international advisers to the INTERYem Family Medicine forum
Dr Saleh Ahmed
CCG lead for Bedfordshire who has also worked extensive in family medicine work in low resource settings
Dr Justin Burdon
Primary Care Dean for HEENE (HEENE- Health Education England North East, the organisation which is responsible for all the postgraduate training for doctors and dentists in the North East of England)
Dr Akye Esuman
Academic family physician from University of Ghana who has spent the last two decades setting up and refining family medicine training programmes there
Dr Enam Haque
GP partner who has worked extensively in family medicine settings in low resource countries
Prof Mosleh Ismail
Professor of family medicine at Suez University, who was instrumental in setting up the first and only such programme in Yemen (previously added by Prof Ahmed)
Dr Shameq Sayeed
Teacher at Leicester and Oxford Universities, and Trustee of Family Medicine Palestine, who helped set up the family medicine training programme in the West Bank
Dr Thanweer Farqhuar
GP with special interest in international health
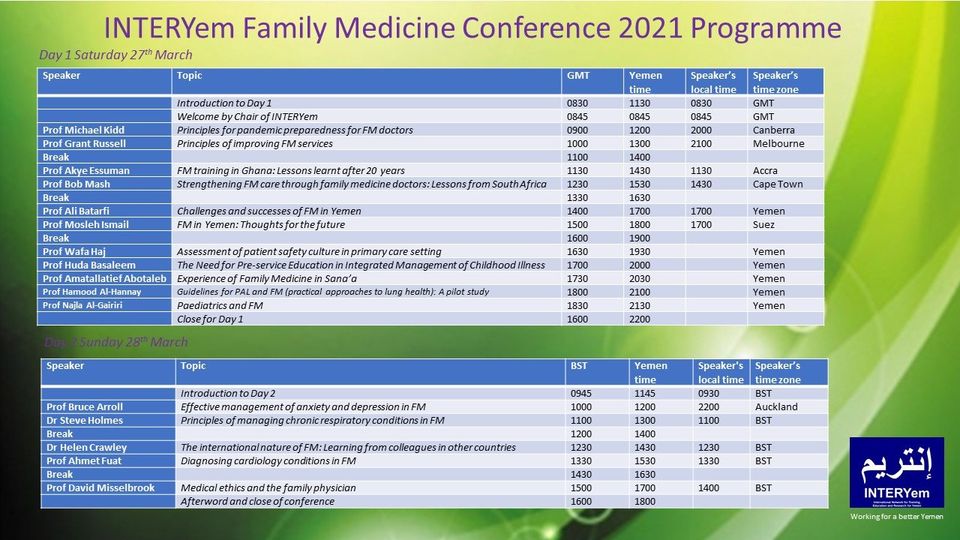
INTERYem Family Medicine Conference 2021
The INTERYem Community and Family Medicine Conference has several objectives. Foremost is the desire to provide an update for FM practitioners, or an overview for those new to the field. Furthermore, the conference will provide an opportunity to exchange information by practitioners and academics in FM from several countries, and this interplay will allow seeds of collaboration to exist. Finally, the FM conference will allow for the initiation of considering where the gaps in training in FM maybe amongst Yemen’s FM HCPs and help us to consider how to work with Yemeni colleagues to fill those gaps.
Conference Information
Delivered Online on 27th and 28th March.
Delivered through the INTERYem Devolved Model.
Live at lecture theatres of medical schools and major hospitals throughout Yemen.
Alternative online means of taking part will be available.
Anticipated Audience
- Non-Governmental Organisations with Family Medicine Dimensions
- Health Policy Designers
- Non-FM HCPs who have an interest in the topics discussed
- Non-FM HCPs who wish to acquire recognition for CCE (continuing clinical education)
- Non-FM HCPs who wish to acquire recognition for CCE (continuing clinical education)
- Community Medicine Doctors
- Family Medicine Doctors
- Allied Public Health Professionals
- Students Interested in Family Medicine
Invited Speakers
Prof. Bruce Arrol
Effective management of common mental health conditions in Yemen’s primary care
Prof Ahmet Fuat
Diagnosing cardiology problems in family medicine
Prof Ali Batarfi
Family medicine training in Yemen
Prof. Akye Essuman
Family medicine residency training in Ghana after 20 years: Potential lessons for Yemen
Prof. Michael Kidd
Principles for pandemic preparedness for community and family doctors
Prof Mosleh Ismail
Community and family medicine training
Conference Programme
Certificates
Certificates of Attendance will be awarded to those who register and attend the whole conference. You will be asked to complete a feedback form before receiving your certificate